Professional boundaries are the borders or limits that a nurse sets to protect themselves and their clients from developing unprofessional, unethical, confusing, or conflicting relationships. Boundaries are required when developing therapeutic relationships with clients due to the personal nature of nursing care.
Boundaries sit on a continuum that ranges from under-involvement to over-involvement. The zone of the therapeutic relationship is in the middle. Client harm can occur at either end of the continuum. Appropriate professional boundaries create a zone that allows for a safe, effective relationship between the nurse and the client.


As the nurse, you are always responsible for establishing and maintaining appropriate boundaries, regardless of how a client behaves. Some boundaries are clear-cut; others are less clear and require your professional judgment. It’s important that you recognize when a professional relationship is moving out of the zone of helpfulness and into the nonprofessional zone, and that you take immediate action.
Boundary crossings and violations
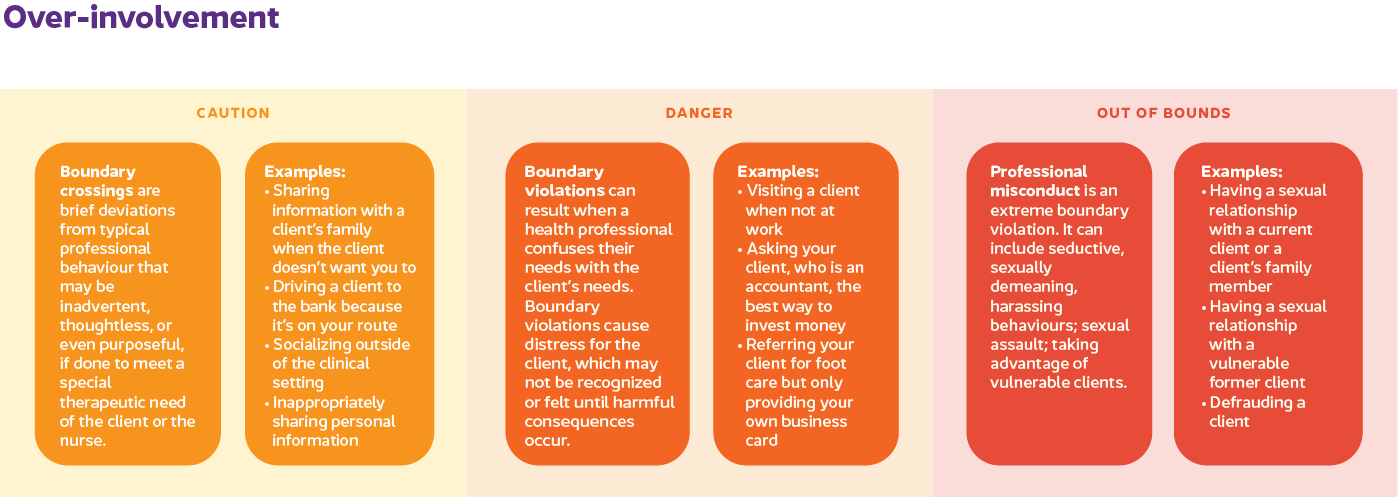
Inappropriate professional behaviours can be separated into three categories:
- Boundary crossing
- Boundary violation
- Sexual misconduct
Some minor behaviours may appear harmless but can lead to behaviour patterns that indicate the nurse-client relationship is no longer in the therapeutic zone.
Warning signs of boundary issues
Signs of inappropriate behaviour can be subtle; however, these signs indicate a need to reflect on the nurse-client relationship and clarify boundaries. The following behaviours can signal potential boundary issues.
- Over-involvement with a client
-
- Thinking about a client frequently when you're away from work
- Giving preferential care or time to the client and putting their care needs above others
- Feeling responsible for a client's outcomes or lack of progress and being irritated by treatment delays or barriers
- Having more physical contact with a client than is required or appropriate
- Spending breaks or time off with a client, seeking social contact, and providing personal information such as your email address or phone number
- Participating in personal conversations, flirtations, off-color jokes, or sexual innuendos
- Feeling a sense of excitement, longing, romantic or sexual thoughts related to a client
- Hiding your relationship with a client from others
- Receiving feedback from others that your behaviour is overly familiar or intrusive
- Refusing to transfer care of a client to another provider when therapeutically indicated
- Under-involvement with a client
-
- Delaying care or treatment, e.g., waiting to answer a call bell or delaying a needed medication unnecessarily
- Taking short cuts in a client's care, e.g., not providing daily hygiene, skipping a dressing change
- Blaming a client for lack of progress
- Being rough when providing care
- Using disrespectful, demeaning, insulting, or humiliating language or tone
- Inadequately draping a client during a procedure
- Avoiding a client so that it interferes with meeting care needs
- Withholding information that a client needs to make an informed decision
What to do if you see warning signs
Some boundaries are absolute and must never be violated. Others require judgment and careful consideration of the context. Some behaviors, while unacceptable in most contexts, may be acceptable and appropriate in special circumstances.
- Reflect on your situation
-
Maybe you’re uncertain or wondering if you’ve crossed a boundary with your client. Perhaps someone points out how others could view your behaviour. If you’re concerned of a potential boundary issue, take steps to address it right away. Reflecting on the situation and your behavior and exploring concerns can help you understand your own feelings and motives and recognize the effect of your actions on the client. Consulting with a knowledgeable and trusted colleague is an objective place to start.
As a nurse, you are responsible and accountable for your actions and professional conduct. If you’ve breached a professional boundary, you must take steps to restore the boundary appropriately. It may be necessary to withdraw from or end the therapeutic relationship.
Behaviour outside the therapeutic relationship requires intervention and/or reporting to the relevant regulator. If you are unsure if reporting is required, call a BCCNM complaints Intake Advisor for consultation.
Caring for friends and family
In situations where you have both a personal and professional relationship with a client, you are acting in a dual role. When you have a personal relationship with someone, you may find it difficult to be objective enough to have an effective professional relationship. You may have difficulty separating personal feelings, values, and beliefs from your professional and ethical obligations.
BCCNM
recommends that, when possible, nurses avoid dual roles and transfer overall responsibility for care to another health-care provider.
- If you are unable to transfer care or choose to provide some care, you will need to use caution. Ensure:
-
-
All available alternatives are explored with the client and the health-care team.
-
The client is fully informed and consents without feeling pressured or coerced.
-
You make it clear to everyone concerned (the client, client’s significant others, other health-care team members, and yourself) when you are acting in a personal role and when you are acting in your professional role.
-
You continue to meet all professional and ethical standards (especially privacy and confidentiality, consent, documentation, conflict of interest, duty to provide care).
-
You follow any employer/organizational policies related to caring for friends and family.
- How to maintain a therapeutic nurse-client relationship
-
-
Dress appropriately for the client context.
-
Be clear, in your mind and with the client/family, about your professional role and responsibilities when at work by establishing and maintaining the professional boundaries in your relationships with the client/family.
-
Ensure your behaviour meets the needs and best interest of the client.
-
Be fair and consistent with each client by ensuring your care is objective and won't be seen as favouritism.
-
Self-disclose only for therapeutic purposes and only if it doesn't adversely affect the client's care and well-being.
-
Explain your actions and obtain client consent before initiating any activities.
-
Ensure you are communicating with a client's family or friends only as allowed by the client and as permitted by law.
-
Acknowledge your own emotional response to the client and take steps to resolve it.
-
Maintain an appropriate emotional distance to ensure objectivity, without becoming disengaged.
-
Provide clients with adequate privacy.
-
Touch clients only in a manner consistent with accepted standards of nursing practice.
-
Don't discuss any personal, sexual, or romantic activities, relationships, or fantasies with clients or others in the work setting.
-
Don't touch a client without establishing therapeutic intent and considering context, appropriateness, and client permission.